Austerity can kill: public health authorities obstruct new treatments
Spanish patients and families are being denied access to expensive drugs Medicines are approved but hospital authorities resort to bureaucratic ploys


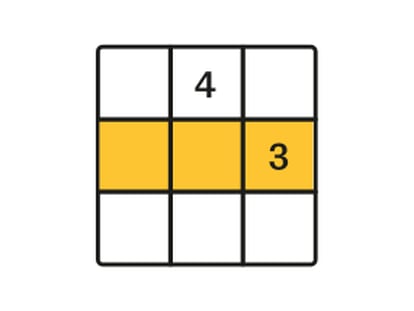
When this newspaper first talked to 47-year-old Xabier Etxeberria in June, he was fighting to get the Basque public health system, Osakidetza, to give him the treatment most likely to cure his hepatitis C. A month earlier, he had filed a written request for the triple therapy, claiming it was being denied to him for "economic reasons." When Osakidetza replied, it basically agreed with him: because his liver still had a Grade 2 fibrosis, the treatment could not be administered since the policy is to reserve this triple medication for more advanced cases, with Grade 4 being the equivalent of cirrhosis.
Etxeberria, a father of three who works as a monitor for people with psychiatric conditions, informed EL PAÍS last week that he is finally on the triple therapy, following a treatment that lasts between six and 12 months and costs 30,000 euros. This treatment increases recovery rates by between 45 and 75 percent.
So this should be good news, right? Not really. What happened is that between June and now, as he waited "feeling completely exhausted with no energy," Etxeberria's liver got worse and he now has Grade 3 fibrosis. So now Osakidetza is paying for his treatment. In their reply of last June, health system officials justified their initial refusal with the following statement: "Impossibility of addressing your treatment at the present time."
Scientific societies and patient associations agree: it is getting increasingly hard to access the kinds of medication that doctors feel would be best for their patients when this medication happens to be very expensive because it is either new on the market or aimed at rare diseases. It happens with cancer treatments, but also with the new oral anticoagulants used for thrombotic disorders. And it happens with the new treatment for hepatitis C, which almost doubles the cure rate of the current therapy.
Is a medication expensive if it prevents a €150,000 transplant?"
"Expensive or cheap, it depends on what you're measuring. If medication can prevent a transplant, which costs 150,000 euros, or cancer or cirrhosis..," notes José Luis Calleja, a lecturer at Madrid's Autónoma University and deputy head of the gastroenterology department at Puerta de Hierro hospital. There are 900,000 people living with hepatitis C in Spain.
"There is a lot of talk about prioritizing, but this word is always a doubled-edged sword, because it does not mean prohibiting. In practice, many regional governments have been using it to postpone administration of this drug," adds Calleja, who is also secretary of the Spanish Association for Liver Studies (AEEH) and helped draft a report on the therapeutic usefulness of the triple therapy for the Spanish Prescription Drug Agency (Aemps). Experts concluded that it was effective for Grade 2, 3 and 4 patients. The same day this report was issued, another document was released: a "prioritization annex" that had not been signed by the specialists, and which stated that this therapy should only be administered to Grade 2 patients "exceptionally." This, says Calleja, was the first filter. Problems accessing expensive medication begin at Aemps, and continue with regional authorities and local hospitals, all experts consulted by this newspaper agree.
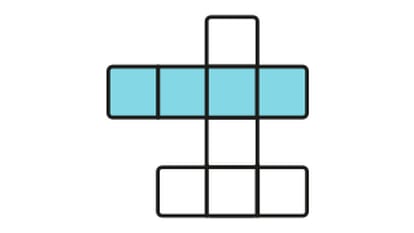
The Spanish Society for Hematology and Hemotherapy (SEHH) is one of the most vocal critics of this complex situation. President Carmen Burgaleta explains that difficulties accessing the best medication are "constant" and have become more acute during the last year. To this must be added the problem of inequity. The same patient could get the go-ahead for a given treatment in one region but not in another; or even worse, get a yes in one hospital but a no at a different hospital just two kilometers away.
But the main obstacle is the Health Ministry, Burgaleta says. "We are concerned about growing delays getting new drugs authorized." A case in point: Ruxolitinib, a drug that hematologists have been waiting for "with excitement" for the last few years in order to provide better treatment for patients with myelofibrosis, a rare bone marrow disease. "Turns out it's been approved everywhere in Europe except for Italy and Spain," says Burgaleta.
We are concerned about growing delays getting new drugs authorized"
Physicians are pretty certain that if the veteran drug Sintrom (whose active ingredient is acenocoumarol) is still the anticoagulant of choice for patients with cardiac arrhythmia at risk of an ictus, that is because of budget restrictions. The new oral anticoagulants Dabigatran, Rivaroxaban and Apixaban are equally efficient in preventing an ictus, but are easier on the patients because of the lower risk of hemorrhaging and fewer required visits to the doctor. The thing is, Sintrom costs three euros a month, while the others come with a price tag of nearly 90 euros.
"When you analyze sales and the penetration rate of the new drugs, you realize that the progression has not been what one might have expected," says Vicente Bertomeu, president of the Spanish Cardiology Society (SEC). "There are health areas where they are practically never prescribed," he adds.
In Spain, these drugs require a special authorization from Medical Inspection. "One out of three patients who take Sintrom is not under proper control and might be a good candidate for the new types of medication," explains José María Lobos-Bejarano, a family doctor and coordinator of the Cardiovascular Group at the Spanish Society for Family and Community Medicine (Semfyc). "It makes no sense, now that we have the new anticoagulants, to run into these hurdles of a purely economic nature. Many family doctors keep up treatment with Sintrom, the way they did when there was no alternative, and that is not right. In some regions, primary care physicians are not allowed to prescribe these drugs, and patients need to be referred to a specialist, delaying treatment. It acts as a deterrent and represents a missed opportunity. On our recommendation, some patients pay for their own treatment. Studies have shown that [the new drugs] reduce ischemic stroke by 35 percent more than Sintrom," he adds.
The half a million members of the Federation of Anticoagulated Patients (Feasan) also report major differences between the regional health services, and even between hospitals. This group talks about "major inequality" because there are regions such as Castilla y León, Castilla-La Mancha, Murcia, the Canary Islands and Aragon where the primary care physician cannot prescribe the treatment. "Although the ministry published a document unifying criteria, some regions have incorporated recommendations that add more filters to access, such as Catalonia, Castilla y León and Madrid."
These drugs reduce ischemic strokes but physicians stick with Sintrom"
Twelve-year-old Fouad is too young to know about mucopolysaccharidosis, a group of rare diseases causing cellular damage because of a malfunctioning enzyme. There are around 50 people with it in all of Spain. But he suffers from one of its forms, the Hurler-Scheie Syndrome. His mother, Houssnia el Khadiri, explains that two of her four children (including five-year-old Fadwa) suffer from this genetic disease. Although Fouad was diagnosed four years ago - he cannot move his arms much, has cataracts and is shorter than other children his age - he is still not getting the enzymatic treatment that would relieve his symptoms. Specialists consulted by this newspaper were at a loss to explain why it has not been approved.
So is El Khadiri, who has visited one health center after another trying to get the necessary treatment for her children. Jordi Cruz, president of the Mucopolysaccharidosis Association of Spain, is convinced that it is because the treatment costs thousands of euros.
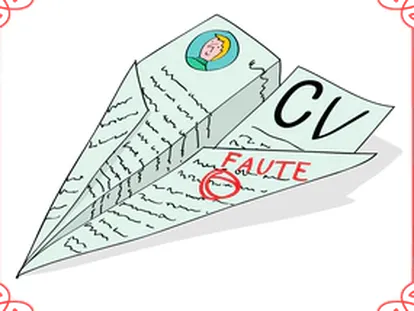
"It seems clear to me that if we were not in the current economic situation, this would not be happening," he says. The fact remains that La Paz hospital in Madrid, which treated both children at its genetics department, never approved the treatment. Their case was referred to the hospital's Committee for Compassionate Use and Special Medication, which in turn deflected it on to the Madrid regional department of health. El Khadiri has yet to receive a specific reply or a document of any kind officially refusing to provide the treatment.
Last Friday, following a call from EL PAÍS, a spokeswoman said that Fouad will be getting his treatment next week. They said the same thing in July 2012 to another media outlet that also covered the case, Fouad's mother recalls. But they never kept their word.
Fouad's mother has yet to receive an official refusal to provide treatment
"With treatment, these children could lead normal lives. But everyone just washes their hands," sighs Cruz.
Just a few days ago, the Galician health service, Sergas, was forced by a court ruling to finance an expensive drug called Eculizumab that relieves the symptoms of people with an extremely rare disease of the blood called Paroxysmal nocturnal hemoglobinuria (PNH).
"Following the ruling, three or four more patients will be receiving the medication," says Cruz, who also presides the PNH Association. "For the 7,000 existing rare diseases, many of which are serious, there are only 55 drugs. My daughter has Sanfilippo Syndrome
[another form of mucopolysaccharidosis] and there is no medication for her. Is it so complicated to treat people whose condition has an associated drug? Why do they approve drugs only to later create all kinds of hurdles?"
"It took the ministry 11 months to get the committee that approves new medication and prices to meet," says Albert Jovell, a physician and president of the Spanish Patient Forum. "This committee is highly influenced by the Economy Ministry, because the Health Ministry might give the green light, but it's the regions who pay. They try to delay the moment when hospitals start handing out the drugs, or else they run patients through strict selection processes. And as the health budget shrinks, this trend has been on the rise. Doctors have very little leeway when it comes to writing out prescriptions, and no matter how well-informed the patients, they don't realize what is going on."
Jovell feels that the greatest trouble lies with treatments for cancer, hepatitis C, rheumatoid arthritis and multiple sclerosis.
Belinda Lozoya, 29, has just found out that the 18 months that she's been on a waiting list to get an insulin pump implant may have been for nothing. Because of her age, her profession - she is a nurse and works in shifts - and her two decades as a diabetic, she is a good candidate for this device. That is what her endocrinologist at Henares Hospital in Madrid told her when he referred her to La Paz in March 2012 for the implant because her diabetes was not under proper control. Since then, she has been a patient at the endocrinology department in this hospital. But now that her turn was coming up, the hospital is refusing to finance the pump and the ancillary equipment. It alleges that Lozoya falls into a different health area because of her home address. But Madrid approved the single health area in 2009 and advertised that patients could freely choose between centers throughout the region. In practice, as Lozoya knows, hospitals try to stick to their reduced budgets by sending patients back to their local centers. "I am left in no man's land," she notes. "Bureaucratic and financial problems at the hospital should not be an issue for a patient who needs a treatment."
The Health Ministry asserts that it is working to unify criteria at all Spanish hospitals and denies that it is taking longer than necessary in getting innovative drugs approved. It also suggests that the prices set by some labs are impossible. Meanwhile, patients are running into increasingly large hurdles that they are often unaware even exist.
Less spending = higher cancer mortality
Health spending has a direct correlation with the possibility of surviving cancer. The more a government spends on health, the lower the cancer mortality rate. This link is even more evident in the case of breast cancer, according to a study published in the journal Annals of Oncology. The results of the research were presented at the European Cancer Congress held recently in Amsterdam.
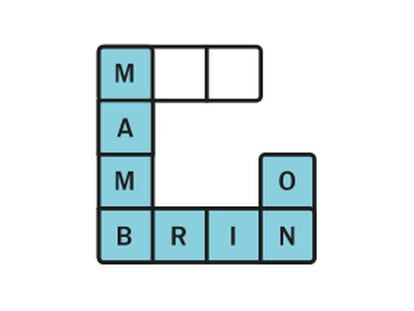
Its authors used World Health Organization data on cancer incidence and mortality, and compared it with per capita health spending in 27 EU countries (Croatia, which has just joined, was not included). The result was a strong direct correlation between health spending and cancer survival after a diagnosis. Although the report does not go into the causes of this association, authors suggest that greater spending allows for earlier diagnosis and more efficient, accessible treatment.
Researchers found that in countries that spend around $3,500 (2,588 euros) per person per year, mortality for all cancer types was 45 percent of diagnosed patients. If spending is increased by $500 (369 euros), mortality is reduced by five percent.
"Mortality falls the more governments invest in health, although as spending increases, marginal gains in mortality are reduced," explained the main author of the study, Felipe Ades, an oncologist at the Jules Bordet institute and lecturer at the Free University of Brussels.
The work raised special interest among the Spanish media at the congress. The results make it likely that "austerity policies will cause a rise in cancer mortality," said Ades. This view concurs with that held by the Spanish Society of Medical Oncology, which has stated on several occasions that the spending cuts mean delays in approving the latest treatments.
The figures used in the study date back to 2008 and they do not analyze trends, making it impossible to measure the effect of the crisis. That year Spain ranked 13th in health spending, but that was before the health budget started to drop (by five percent in 2010 and another five percent in 2011, according to a report by the Organisation of Economic Co-operation and Development).
The study does not take into consideration other factors that might affect cancer mortality rates, such as genetics, lifestyle, environmental exposure to carcinogens, infections and more. The lower death rates in wealthier countries may also be linked with a greater incidence of early detection. The authors will analyze the data again in 2014.